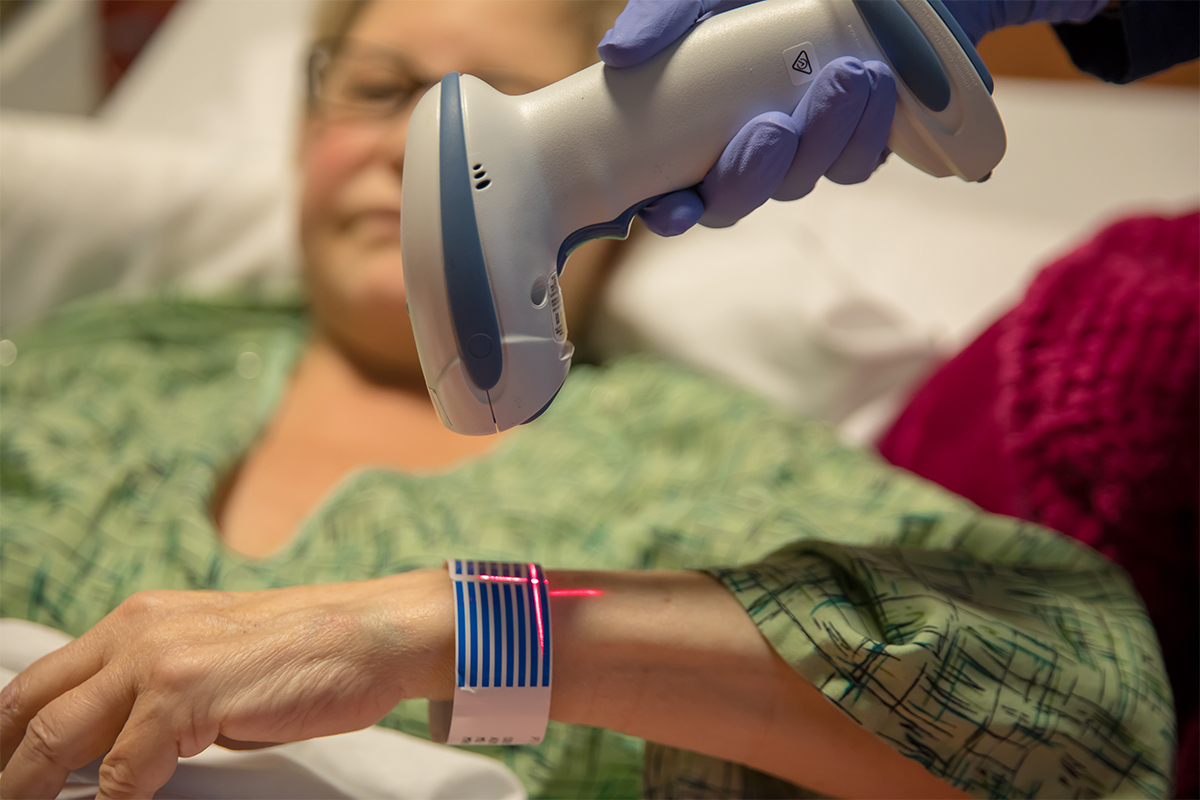
When a patient is admitted to a hospital, a wristband attaches them to the vast health care system. When that system works well, the patient gets the necessary care in an effective manner. But if the system doesn’t work well, the consequences can be inconvenience, inadequate care, or even life and death.
Italia Passanante, ’21, M.A. ’22 and Ryan Romualdo, ’21, M.A. ’22, began their assignment for the Healthcare Systems Engineering Program at a medium-sized hospital with two clinics and saw a problem right away: not all patients were getting wristbands. They had gathered a list of protocols from the hospital administrators, yet the first patient they observed didn’t have a wristband and the second one did. The wristbands, with a unique barcode, said Passanante, identify each patient and confirm the course of treatment and procedures for that patient. Missing wristbands introduce a measure of doubt and inaccuracy that could have dire results. A patient could even be lost to the system.
“Italia and I proposed a series of solutions to reduce the biopsy wristband error rate,” said Romualdo. “The main solution was setting a standardized workflow for all ambulatory clinics that included a wristband for every patient and making sure multiple identifications were taken throughout the process. Moreover, the standardized workflow included printed labels for the biopsy specimens, as they were handwritten prior to this.”
The comprehensive approach to health care systems is what makes Loyola Marymount University’s Health Care Systems Engineering (HSE) Program in the Frank R. Seaver College of Science and Engineering an innovative, and effective training program focused on impactful solutions that will advance healthcare for everyone. HSE — the only program of its kind in Southern California — educates current and future health care professionals on the principles of systems engineering to help optimally manage the complexities and challenges facing health care today.
David Quam, M.D., a 1982 LMU graduate who returned to campus in May 2022 to become director of the Healthcare Systems Engineering program, said one of the focal points of the program is “training people to be defragmenters.” He said, “Fragmentation in the system can lead to medical errors. The discipline with engineering can improve quality and reduce waste, certainly, but it can also increase patient care. We want LMU grads to have immediate effect.”
Healthcare Systems Engineering began as a certificate program for professionals that focused on Lean Systems principles. It is now a Master of Science degree program with an additional option for undergraduates – a 4+1 that prepares students to earn an M.S. in a year – a dual M.S./MBA degree program, and the certificate in lean health care.
Passanante and Romualdo graduated from the 4+1 program; Passanante is beginning her veterinary program in Tennessee in the fall; Romualdo is applying his systems knowledge at UCLA Medical Center with a patient identification company.
Systems engineering is defined as an interdisciplinary field of engineering and engineering management that focuses on how to design, integrate, and manage complex systems over their life cycles. When applied to health care, it takes in the panoply of concerns, from billing to stocking equipment to patient safety and privacy to delivery of care, and everything that implies.
Quam, who served as a primary care family medicine physician and held senior executive-level positions in Kaiser Permanente’s Southern California region, said that systems engineering emphasizes a thorough analysis of the present state of a health care entity’s processes and outcomes, taking an across-the-board look at how it works, from bottom to top. Though the systems are the primary concern, “All students take a personal interest in patients’ welfare. It all comes down to one patient at a time and our students learn an understanding of all departments in a health organization and how they work together.”
A distinctive feature of the program is that all students are connected to a health care facility or agency where they work on a capstone project to address actual challenges and needs of those institutions. LMU HSE has close relationships with local medical organizations, which benefits the program on many levels: sharing faculty, providing access for student visits, providing capstone projects to students, and facilitating paths to jobs. The projects are mentored by both an academic advisor and a supporter from the medical institutions. Some projects are paid and others unpaid. There is now an East Coast project being developed.
The purpose of the program is to be immersed in the field to find inefficiencies or wasteful practices. They can then apply the systems engineering principles to devise solutions. A partial list of projects reveals the range of concerns students have been involved in:
- Lean Streamlining and modeling of operations in emergency departments, operating rooms, clinics, hospitals, pharmacies, supply chain and administration – reducing waste, cutting costs, giving providers more time for patients and improving quality and work environment;
- Integrating fragmented health care elements into safe and redundant patient-focused systems with well-manufactured interfaces;
- Managing population health, telemedicine, home care;
- Equity and Diversity in health care;
- Reducing errors and accidents in increasingly complex clinical environments.
- Improving the use and interconnectivity of medical devices (“everything is now cross connected”);
- Electronic records and health care enterprise informatics.
“Right systems can save people,” said Quam. “Our goal is to offer high-quality health care proposals to improve quality and the patient experience while reducing disparities.”
Visit the Healthcare Systems Engineering Program website to learn more about the program.



